Scoliosis awareness month is almost upon us, and as usual, we’d like to take the opportunity to draw attention not only to the condition but also to the importance of ongoing research. Scoliosis awareness month, for those who don’t know, takes place in June each year – with International Scoliosis Awareness Day on the last Saturday of each June.
While Scoliosis awareness day is a great opportunity for fund and awareness-raising events, National Scoliosis Awareness Month runs throughout June and aims, in particular, to highlight the growing need for education, early detection and awareness to the public about scoliosis and its prevalence within the community.
According to the scoliosis research society, the organisers of National Scoliosis Awareness Month, its official objectives are:
- Using the results from the BrAIST Study, highlight the importance of early detection and the effectiveness of bracing as early, non-operative care.
- Increase public awareness of scoliosis and related spinal conditions through educational and advocacy campaigns of local activities, and community events during the month of June.
- Unite scoliosis patients, families, physicians, and clinicians in a collaborative partnership that educate, and advocate, for patient care, patient screening, patient privacy, and patient protection
- Build networks of community collaborations and alliances to help sustain and grow the campaign[1]
It’s the BrAIST study – an important landmark for scoliosis research and treatment which we’d like to discuss today.
The BrAIST study
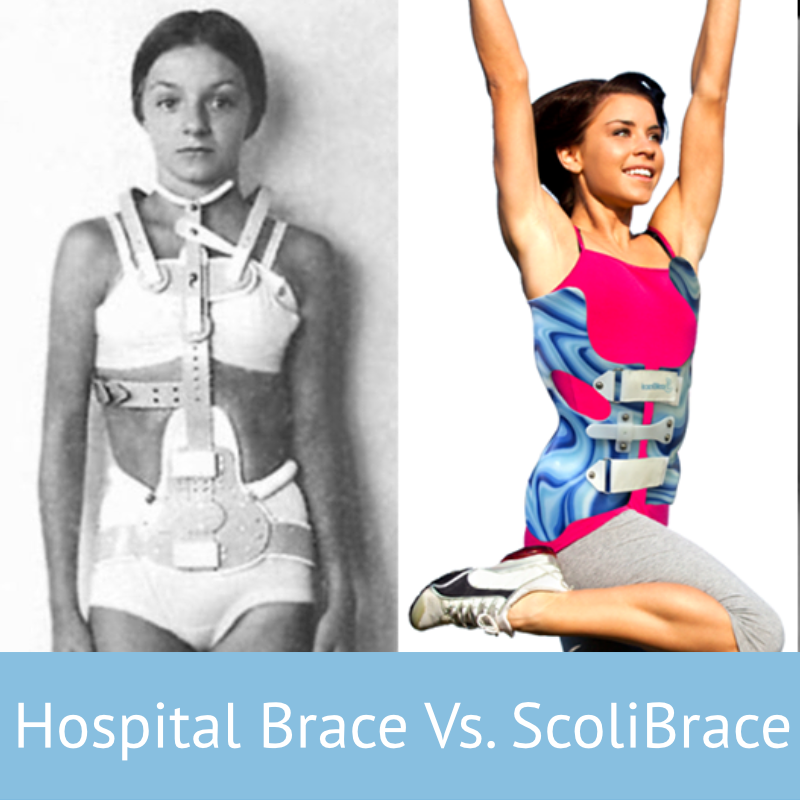
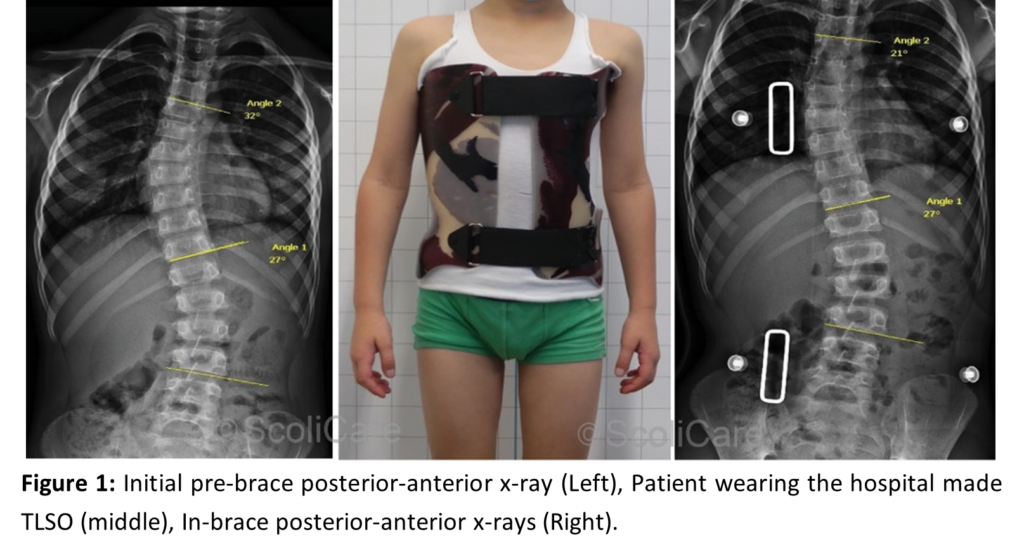
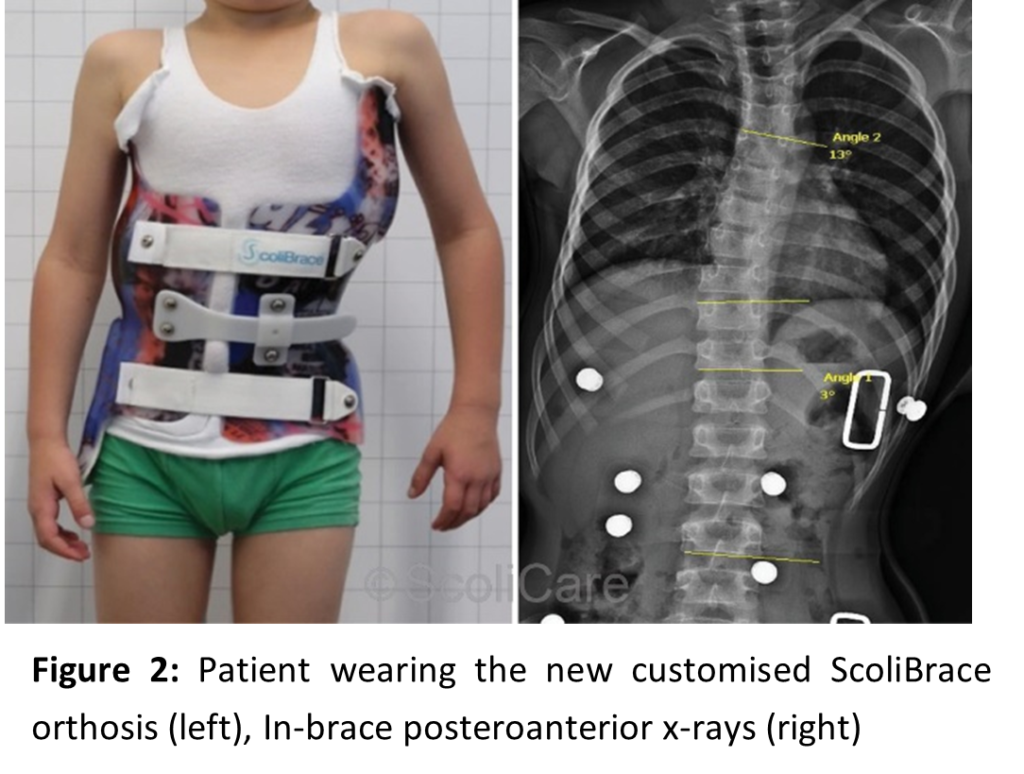
The BrAIST study, overseen by Dr Stuart Weinstein and published in 2013, was perhaps the most impactful study showing the efficacy of bracing in treating scoliosis cases. In short, the study proved that bracing of adolescents with moderate scoliosis was an effective treatment in the reduction of the number of patients who advance to the need for surgery. In addition, a dose-response was found between the number of hours of brace wear and the success rate of bracing – which is to say, there’s a strong relationship between how long a brace is worn, and how effective the treatment is. Both are critical points when considering the value of scoliosis bracing as a whole.[2]
Unlike many of the smaller studies which inform our understanding of scoliosis and best practice in treating it, the BrAIST study was coordinated between several medical centres, and allowed the highest level of medical study, a randomized clinical trial, to be undertaken. To answer the question of whether bracing is effective in growing children and adolescents with curves.
During the study, 242 patients with curves between 20 – 40 degrees participated. Patients in the bracing group were assigned to wear a brace 18 hours per day (a typical bracing prescription). A special monitor was embedded in the brace to keep track of how long it was used per day. Patients in the observation-only group received no additional treatment. The endpoint of the study was “treatment failure” defined as progression of the scoliosis to 50 degrees or “treatment success” when skeletal maturity was reached without progression to 50 degrees.
Across the survey group, 72% of brace wearers avoided surgical recommendations, but only 48% of patients in the observational group did the same. Furthermore, however, it was also shown that patients who complied fully with their bracing instructions, and wore the brace for 13 hours or more was greater than 90%, showing both that the amount of time the brace is worn is very important and that the results we can expect with solid compliance are fantastic indeed. The study, therefore, provided strong evidence to the value of brace treatment for those adolescents at high risk of progression of surgery.
Why the BrAIST study matters.
The BrAIST study was notable due to its size – a large sample set, its nature – a fully randomised clinical trial and the credentials of its authors – a range of expert Doctors. The impact of the BrAIST study was therefore to provide solid evidence not only for non-surgical treatment but also against the “wait and see” attitude which has existed towards scoliosis for decades.
In the past, the value of a screening examination for scoliosis has been debated due to inconclusive evidence of the success of non-operative treatment for scoliosis – simply put, without strong evidence to show it’s possible to avoid surgery, why screen, and why bother?
Thanks to the BrAIST study, this is no longer true. It shows that early screening and non-surgical treatment may reduce the number of patients who progress to surgery and, therefore, could serve as a potential cost saving for the health care system and of great benefit to patients. According to the study, Policy statements from professional organizations and governmental agencies regarding scoliosis screening in school programs and primary care settings will need to be reassessed in order to identify at-risk patients who will benefit from bracing for scoliosis[3].
And it’s this final point that highlights why scoliosis awareness month and the BrAIST study now matter more than ever – it’s 2021, and there’s no sign of the UK government even considering screening in schools for scoliosis, and, despite many organisations best efforts, the majority of people are still unaware of scoliosis, and it’s possible treatments.
That’s why this scoliosis awareness month, we invite you to help us spread the word – and, for your own knowledge, take just a moment to read the conclusions from the BrAIST study – you can find it here and read the abstract in about 3 minutes.
Over the next month, we’ll be posting articles about different kinds of scoliosis, how to spot them and what the treatment options could be – keep an eye out and help us to raise awareness throughout June!
[1] https://www.srs.org/patients-and-families/additional-scoliosis-resources/scoliosis-awareness-month
[2] Stuart L. Weinstein, M.D., Lori A. Dolan, Ph.D., James G. Wright, M.D., M.P.H., and Matthew B. Dobbs, M.D. Effects of Bracing in Adolescents with Idiopathic Scoliosis, N Engl J Med 2013; 369:1512-1521
[3] Stuart L. Weinstein, M.D., Lori A. Dolan, Ph.D., James G. Wright, M.D., M.P.H., and Matthew B. Dobbs, M.D. Effects of Bracing in Adolescents with Idiopathic Scoliosis, N Engl J Med 2013; 369:1512-1521