Degenerative (sometimes called De-Novo) scoliosis is one of two main types of adult scoliosis. De-Novo roughly means “new” so degenerative scoliosis is a type of scoliosis which develops over time as a result of degeneration in the spine. The other kind of adult scoliosis is known as Adolescent Scoliosis in Adult (ASA) – and refers to scoliosis which started at a younger age, but was not treated (or was not treated successfully).
What is De-Novo scoliosis?
Degenerative scoliosis is fundamentally due to wear and tear on the spine, but it is also strongly associated with a variety of conditions. Osteoporosis, degenerative disc disease, compression fractures and spinal canal stenosis have all been implicated in the development of degenerative scoliosis.
Since De-Novo scoliosis is a consequence of spinal degeneration with age, it rarely presents before 40 years of age – although, in patients with no known history of scoliosis, differentiation from degenerative idiopathic scoliosis may be difficult. It is thought that as many as 40% of over 60’s suffer from de-novo scoliosis.[1]
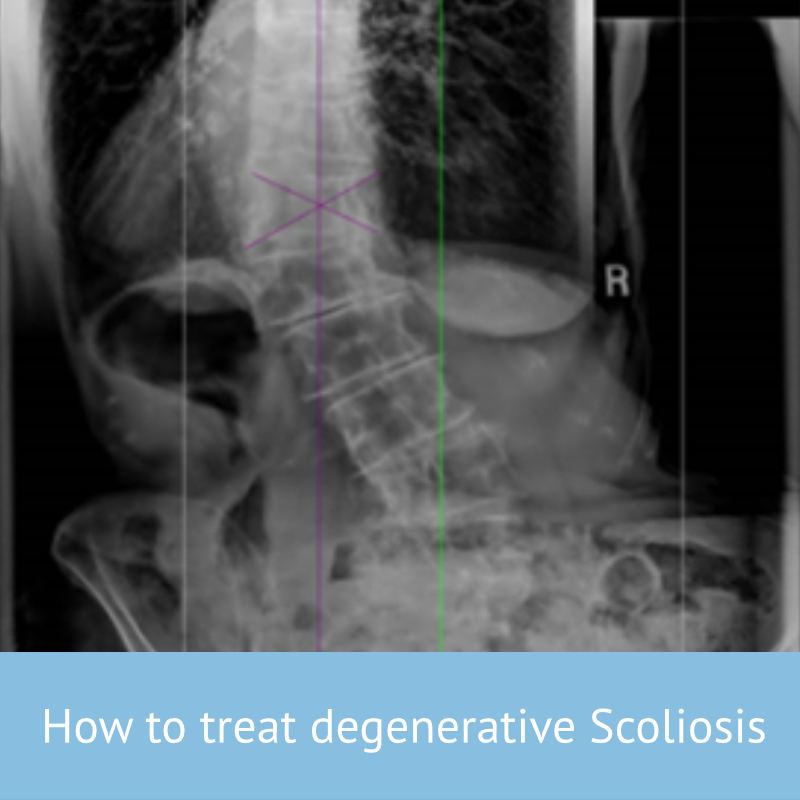
How is De-Novo scoliosis diagnosed?
While most forms of scoliosis are not usually associated with severe pain, De-novo scoliosis is often discovered as the result of a back-pain investigation. Patients with degenerative De-Novo scoliosis typically present with complaints ranging from debilitating back or lower extremity pain to spinal imbalances, as well as as a response to incidental findings on lumbar radiographs. As usual scoliosis will be diagnosed by a combination of physical examination and X-ray or imaging techniques. In the case of De-Novo scoliosis, a thorough examination of the patient’s medical history will help to determine any underlying condition which is implicated in the development of scoliosis.
Counter-intuitively, the pain caused as a result of adult scoliosis is not related to the size of the curve. Several good studies show there is little to no relationship between the size of the curve and the intensity of pain – therefore a 20 degree and a 55-degree curve have the same chance of causing pain in an adult. This means that visual observation is not always sufficient to rule out scoliosis in adults, and professional consultation is the best approach.
Adult scoliosis patients will typically experience significant back pain and stiffness. As spinal degeneration increases, the intervertebral discs become narrowed and nerve compression develops resulting in constant sciatica, pin’s and needle’s, numbness or weakness in the legs. The spinal canal can also become narrowed and result in spinal stenosis where the spinal cord is squeezed so the patient experiences heaviness in the legs, leg pain and difficulty walking
How is De-Novo scoliosis treated?
To achieve effective treatment for adult scoliosis, it is important to be able to differentiate between the symptoms that are caused by the degeneration of the spine as compared to those that are caused by the deformity and its progression.
This means that unless treatment addresses the postural alteration or deformity, the pain and symptoms won’t be improved. This applies to any back-rehabilitation regime, medication course or surgical procedure. Without treatment, we can estimate the increase in curvature to be approximately 0.82° per year, leading to a significant deformity over a period of, say, 10 years.[2]
The good news is that Recent advances in non-surgical treatment have shown significant improvement in terms of reduction of pain and symptoms in those with adult scoliosis. One approach involves the patient learning how to self-correct their abnormal posture, not just strengthen their lower back or core. The most effective approach would be the use of customised brace, such as a ScoliBrace which helps to support the posture in a more comfortable position, pain is reduced (even with part time bracing)[3] and quality of life is improved.
When non-surgical treatment is ineffective, surgery is often the only option, especially when leg pain becomes incapacitating and walking is almost impossible. Unfortunately, surgery at this stage is always complex and with significant risk. This is why it is important to find not only a good spinal surgeon but also one who specialises in scoliosis for the best possible outcome.
[1] ‘Scoliosis in adults aged forty years and older: prevalence and relationship to age, race, and gender‘
Kebaish KM, Neubauer PR, Voros GD, Khoshnevisan MA, Skolasky R, Spine 2011 Apr 20;36(9):731-6.
‘The prevalence and radiological findings in 1347 elderly patients with scoliosis‘
Hong JY, Suh SW, Modi HN, Hur CY, Song HR, Park JH., Journal of bone and joint surgery 2010 Jul;92(7):980-3
[2] Progression risk of idiopathic juvenile scoliosis during pubertal growth, Charles YP, Daures JP, de Rosa V, Diméglio A. Spine 2006 Aug 1;31(17):1933-42.
[3] Scoliosis bracing and exercise for pain management in adults—a case report
Weiss et al, J Phys Ther Sci. 2016 Aug; 28(8): 2404–2407