Do boys get scoliosis? It’s a good question – and it’s one which we don’t hear people ask enough. While it’s certainly true that the majority of scoliosis cases which you’ll hear about in the news are females – and if you know someone with scoliosis, they’re more likely to be female, Males, can, and do get scoliosis.
Scoliosis and Gender
It’s a generally stated fact that scoliosis affects girls more than boys, or, more broadly, it’s frequently noted that about 75% of adolescent idieopathic scoliosis cases are females. Both statements are true – but adolescent idiopathic scoliosis is not the only kind of scoliosis, and 25% is still a large number of people!
To be a little more specific, let’s break the question down – first, scoliosis in children.
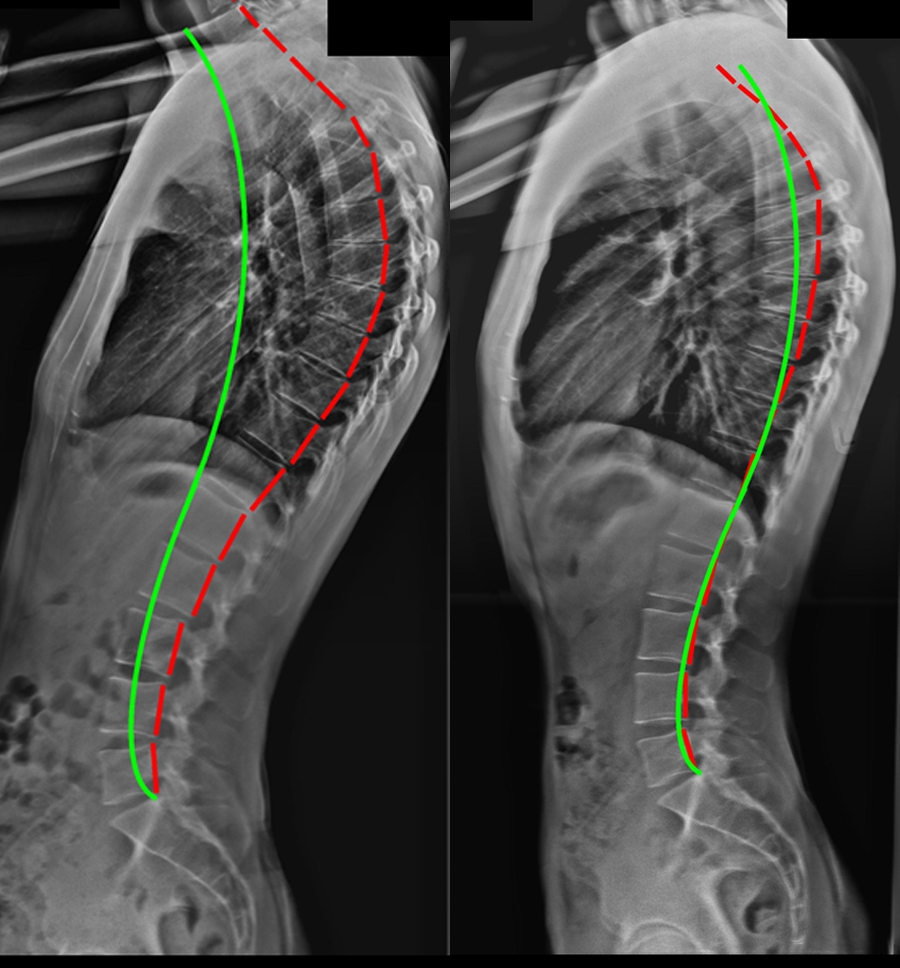
Idiopathic scoliosis is a 3-dimensional distortion of the spine and trunk that occurs in otherwise healthy children. 80% of scoliosis cases in this age group are considered to be “Idiopathic” or “of unknown cause” – scientists are fairly sure that genetics can play a role, but the exact onset of scoliosis Is still not fully understood.
A well-recognised theory about how scoliosis develops in adolescence revolves around asymmetrical growth of the vertebrae which de-stabilises the spine and makes the vertebrae prone to becoming wedged. Wedging of the vertebrae then creates a lateral spinal curve which places uneven loading on the vertebrae and precipitates further asymmetrical growth and progression. It is then thought that spinal cord tension develops as the spine bends and twists and brain function and growth is altered as muscle asymmetry develops.
We break idiopathic scoliosis down further into age groups – and here’s where the numbers get interesting.
Infantile idiopathic scoliosis is the name given to idiopathic scoliosis cases which are diagnosed in children between the ages of 0 to 3 years. Statistically, it is the least common of all forms of idiopathic scoliosis and comprises about 1% of all idiopathic scoliosis in children – while the numbers of overall cases are smaller about 60% of patients are boys.
Juvenile idiopathic scoliosis is diagnosed when scoliosis of the spine is apparent between the ages of 4 and 10. It is less common than adolescent idiopathic scoliosis but more common than infantile. In total, it comprises 10-15% of idiopathic scoliosis cases.
Juvenile scoliosis is also found more often in boys between the ages of 4-6, whereas between 6 and 10 it becomes more common in girls.
Adolescent idiopathic scoliosis is the type which we most frequently hear about – and here is where between 75% and 80% of cases are girls. It is usually noticed around 11-12 years of age in girls and slightly later when diagnosed in boys. AIS is estimated to affect between 3 and 4% of teenagers. In most cases, AIS begins to develop noticeably at the initial onset of puberty and becomes more apparent as is worsens during growth spurts.
While it’s clear that when taken as a whole, girls will tend to make up the majority of scoliosis cases, there are substantial age groups where boys are the most common patients. It’s also critical to understand that while all scoliosis cases should be considered as potentially debilitating, the time available for scoliosis to progress (it typically stops at skeletal maturity) is a huge factor in determining risk. Scoliosis discovered in a 5-year-old boy has considerably more time to progress, than in a 16-year-old girl.
Finally, there’s another common form of scoliosis to consider – affecting a very different age group. Older adults are at considerable risk of another common form of scoliosis, known as “de-novo” (degenerative) scoliosis. De-novo scoliosis is caused by wear and tear to the spinal discs as we age, and is therefore quite common – research suggests that as many as 30% of the over 60’s suffer from scoliosis. Although de-novo scoliosis progresses much more slowly than childhood or adolescent scoliosis it can still have a major impact on quality of life, if not properly treated.[1] De-novo scoliosis affects both males and females – and since such a large percentage of older people can suffer from this condition, there’s a very real argument to be made suggesting that taken over a lifespan, the rates of male and females scoliosis are much closer together than it might seem at first glance.
If you think you may have scoliosis
If you think you may have scoliosis, the advice is simple – regardless of gender, see a scoliosis specialist sooner rather than later. At the UK Scoliosis clinic, we offer in-person consultations at our Essex clinic, as well as online consultations from the comfort of your own home.
[1] ‘Scoliosis in adults aged forty years and older: prevalence and relationship to age, race, and gender‘
Kebaish KM, Neubauer PR, Voros GD, Khoshnevisan MA, Skolasky R, Spine 2011 Apr 20;36(9):731-6.
‘The prevalence and radiological findings in 1347 elderly patients with scoliosis‘
Hong JY, Suh SW, Modi HN, Hur CY, Song HR, Park JH., Journal of bone and joint surgery 2010 Jul;92(7):980-3