While Scoliosis is the main focus of our clinic, we also treat associated spinal conditions such as Hyperkyphosis – it’s a lesser-known condition, not least because Hyperkyphosis is often a progression of “regular” kyphosis, a common condition that can often be managed through approaches targeting postural adjustments, such as chiropractic or physiotherapy.
What is HyperKyphosis
Scoliosis is a condition of the spine that, ideally should not exist (or should be very small in a healthy individual) whereas Kyphosis, in and of itself isn’t a problem as a kyphosis is essential for a healthy spine!
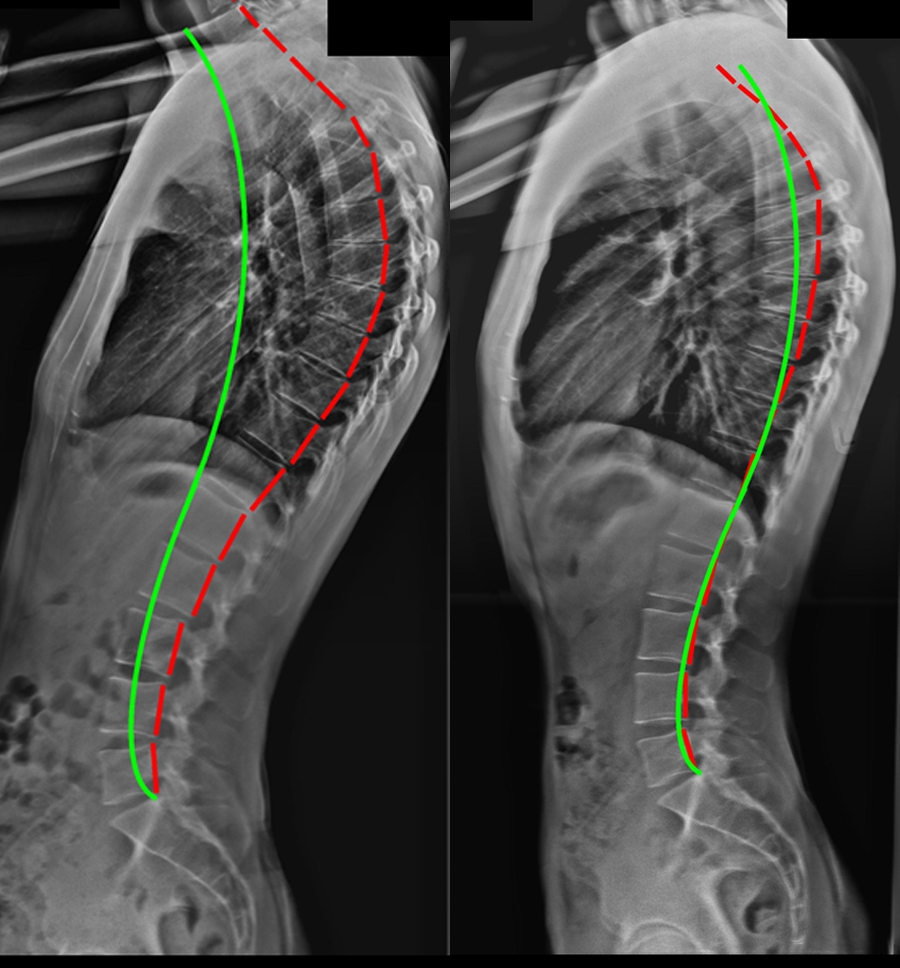
The spine is made up of three main sections: cervical, thoracic, and lumbar. When viewed from the front or back, the spine should appear straight (however in scoliosis it appears curved), and when viewed from the side, it has a slight ‘S’ shape.
This S shape is actually a critical characteristic of the spine which allows it to perform its job. The natural curves of the cervical spine (neck) and lumbar spine (lower back) bend outwards and are referred to as ‘lordosis’. The thoracic spine (middle and upper back) features a curve that bends inwards, and this type of curve is referred to as ‘kyphosis’ – so, kyphosis is in fact, a totally normal condition for the spine to exhibit.
So, if kyphosis is a normal inwards bending of the spine, Hyperkyphosis is said to exist when the kyphotic curve becomes excessive, leading to a rounded appearance of the upper back, a “hunched” posture and often, back pain. We are all individuals with a slightly different spinal and physical makeup, it’s therefore hard to say what an “ideal” kyphotic curve is – for most people a healthy figure is between 20 and 45 degrees, but when a curve falls beyond that healthy range, problems can occur.
When a kyphotic curve exceeds approximately 50 degrees, this is referred to as ‘Hyperkyphosis’ – in many circles, the word “kyphosis” is also often used to mean “Hyperkyphosis” which is unhelpful!
Types of Hyperkyphosis
There are three main types of Hyperkyphosis – broken down by cause, these are postural, congenital and Scheuermann’s
Postural kyphosis is the most common type and is associated with the “hunched” posture we often expect in adolescents. While it’s not true that the use of electronic devices actually causes Hyperkyphosis, the terrible posture this tends to promote most certainly can. Postural kyphosis is the simplest diagnosis to treat, since the condition is caused by poor posture and weakened muscles resulting from it – any treatment approach which aims to address this problematic posture will generally resolve postural Hyperkyphosis.
Congenital Kyphosis is more complex – whereas, in postural kyphosis an individual is born with a normal spine that develops an issue through misuse, a person with congenital kyphosis is born with the condition. There are a number of malformations in the spine which fall under the category of congenital Kyphosis – these include vertebrae not forming properly, or multiple vertebrae fusing together into one solid bone, rather than forming separate and distinct vertebrae.
Some congenital Kyphosis cases may benefit from bracing, but the best treatment will vary considerably depending on the individual.
Finally, Scheuermann’s Kyphosis is a structural condition which affects the way that vertebra develop. In a person with a “normal” spine, vertebrae are rectangular in shape – thus, they sit on top of each other in a fairly level alignment. In patients with Scheuermann’s kyphosis, a number of consecutive vertebrae are more triangular in shape, meaning that they naturally want to curve irrespective of the health of surrounding supporting muscle.
Abnormal spinal curvatures caused by this type of kyphosis are often angular, stiff, sharp, and rigid, which is why this form is more complex to treat and can’t simply be corrected with a change of position. Scheuermann’s is more common in boys and is progressive during growth, which is why proactive treatment is so important.
Kyphosis, which treatment is right for me?
The vast majority of Hyperkyphosis cases tend to be postural in nature, so, while expertise is required to provide a suitable treatment there are many approaches that can help. Chiropractic and physiotherapy are two approaches we utilise at the UK Scoliosis Clinic, but any approach which alters the problematic posture will, over time tend to resolve this condition. It’s also true that many kyphosis cases which are visible, or cause pain do not reach the threshold for Hyperkyphosis – you should, however, look to treat the condition as early as possible, since it will tend to progress without intervention -, even if that only means getting some professional advice on improving your workspace to promote good posture.
Congenital cases and Scheuermann’s kyphosis can often benefit from more specialist treatment through a spinal clinic, like the UK Scoliosis clinic. Spinal bracing, similar to that used for Scoliosis can be appropriate in some circumstances – in others, the best approach may still be a manual therapy coupled with postural work although for more complex cases it’s often worth coordinating this through a specialist centre.